When we hear the word “cancer”, most of us immediately think of adult cancers, the ones at the center of glamorous media campaigns, well-publicized fundraising drives, and focused research efforts, such as breast cancer, colon cancer, prostate cancer, lung cancer, just to name a few. When we hear the words “childhood cancer”, most of us probably think of those same cancers, just in miniature, and assume they have the same causes and the same treatment protocols. In fact, childhood cancers are very, very different than adult cancers, and require very different, specialized treatments.
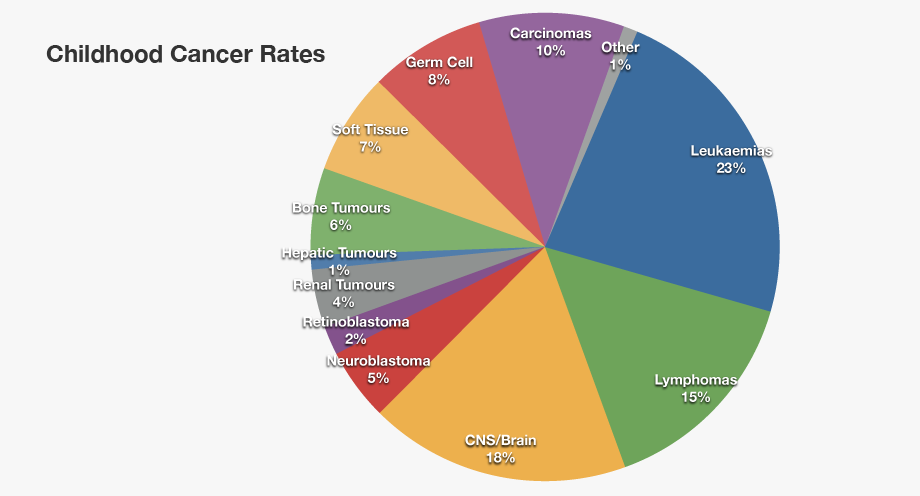
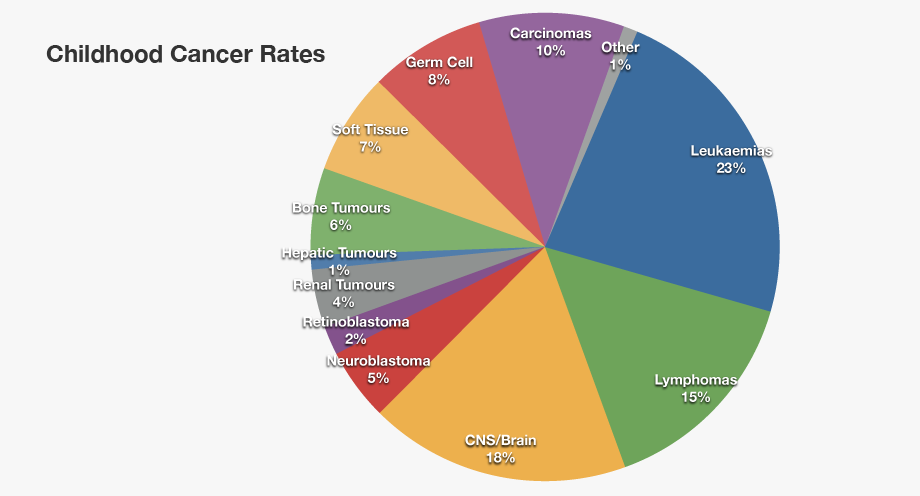
“Childhood cancer” is a general term describing more than 12 different types of cancer, each of which has numerous sub-types, and each of which requires precise treatment protocols tailored to the small, still-developing bodies of children. The American Childhood Cancer Organization is dedicated to raising awareness about the unique challenges presented by childhood cancer, and the desperate need for new and better treatment protocols that will target these dangerous cancers without the permanent and disabling late term effects that are the all-too-common result of treating childhood cancers with drugs developed to cure adult cancers. We encourage you to read about these most common forms of childhood cancer below, and support the ACCO in its mission to improve the lives of children facing this dreaded disease.
Childhood Leukemia
Leukemia is the most common form of childhood cancer, covering more than 30% of all childhood cancers. Leukemia originates in the soft inner part of the bone—the marrow—which is responsible for the development of blood cells. It usually affects the development of white blood cells that are responsible for fighting infection, compromising the body’s ability to fend off disease and heal itself, but leukemia can develop in other types of blood cells as well. The two most common forms of leukemia in children are Acute Lymphocytic Leukemia (ALL) and Acute Myelogenous Leukemia (AML). The good news is that treatments for childhood leukemia have greatly improved in the past decade, and the five-year survival rate is now over 85% for ALL, and over 70% for AML.
Central nervous system and brain tumors
This is the second most widely seen cancer in kids, making up approximately 26% of all childhood cancers. There are several categories of brain tumors and the treatment and prognosis of each of the type is different, depending on a variety of factors including where the tumor is located, the areas of the brain and/or nervous system it is affecting, and how quickly it is growing. It has been observed that children who suffer from such cancer tend to develop tumors in the lower portion of their brain, such as the cerebellum, or the spinal column. Such tumors can cause trouble with object handling, dizziness, blurred vision, vomiting, nausea and headaches.
Neuroblastoma
This type of childhood cancer starts in nerve cells inside a developing fetus or embryo, and grows into tumors in nerve clusters. While neuroblastoma can develop in any part of the body, it is most commonly found in the abdomen. It is by far the most common form of cancer in infants, and is usually diagnosed between the ages of 1 and 2, although can be diagnosed in children as old as 10. Unfortunately, early diagnosis is very difficult, and in 2 out of 3 cases, the disease has already spread to the lymph nodes by the time of diagnosis.
Wilms Tumor
Wilms Tumor develops in or near one or both kidneys, and may even begin developing while the children is still in the womb. It is usually diagnosed in children between the ages of 3 and 4 years old, and is rarely seen in kids above 6 years old. It usually shows as a lump or swelling in the abdomen. The child may often have other symptoms such as poor appetite, nausea, pain, and fever. Wilms Tumor contributes to about 5% of cancers in children.
Bone cancers
Bone cancers in children usually fall into one of two main groups. The most common form—Osteosarcoma—develops in the bones around the knees or near the ends of the long bones of the legs, although it does occasionally occur in the arm bone near the shoulder, the hip bone, or even the jaw. Ewing sarcoma (Ewing family of tumors) is a less common form of bone cancer, usually forming in the pelvis, the chest wall (ribs and shoulder blades), or the middle of the long bones of the leg. While both forms of bone cancer are most commonly diagnosed in teenagers and older children, they can be found in younger children as well. There are some commonalities between these two types of bone cancer, but they respond differently to current treatment protocols.
If you are interested in learning more about these or other forms of childhood cancer, if you would like to know more about the critical need for additional research into the causes and appropriate treatments for childhood cancer, or you would like to support the ACCO’s mission to support all children coping with cancer or its long-term effects and their families, we encourage you to visit www.acco.org to find out how you can help!
For more information about the American Childhood Cancer Organization call 855.858.2226 or visit:




 Grace loves to be crafty; she made a sign for the children to sign and date which says “Last Day of Chemo.” Throughout her treatment, she decided to paint pictures to brighten the nurses and the children’s days. When losing her hair became a reality, Grace decided to throw a party and shave her head. Grace’s brother and her best friend joined her in shaving their heads as well.
Grace loves to be crafty; she made a sign for the children to sign and date which says “Last Day of Chemo.” Throughout her treatment, she decided to paint pictures to brighten the nurses and the children’s days. When losing her hair became a reality, Grace decided to throw a party and shave her head. Grace’s brother and her best friend joined her in shaving their heads as well. lking to people about this part of her journey and is focused on helping others. Grace plans on learning more about oncology. She is excited for the future and can’t wait for her hair to start growing back!
lking to people about this part of her journey and is focused on helping others. Grace plans on learning more about oncology. She is excited for the future and can’t wait for her hair to start growing back! 

 The good news is that there have been tremendous advancements in the treatment procedures for many forms of childhood cancer, and five-year survival rates for some types of cancer have risen dramatically in recent years. However, both chemotherapy and radiation therapy, the two most common forms of treatment, involve intensive levels of both medication and energy that can target healthy cells in addition to killing cancerous cells. Unfortunately, these treatments may, and often do, cause severe health-related problems later on. These are called “late term effects”. While helping your child cope with the short-term and often extremely difficult side effects during or immediately after treatment often takes first priority, it is important to be aware of the types of health problems that may not develop for months or even years. And as the survival rate continues to improve, but treatment still relies on smaller dosages of adult protocols, more and more children will suffer from “late term effects” throughout the remainder of their lives.
The good news is that there have been tremendous advancements in the treatment procedures for many forms of childhood cancer, and five-year survival rates for some types of cancer have risen dramatically in recent years. However, both chemotherapy and radiation therapy, the two most common forms of treatment, involve intensive levels of both medication and energy that can target healthy cells in addition to killing cancerous cells. Unfortunately, these treatments may, and often do, cause severe health-related problems later on. These are called “late term effects”. While helping your child cope with the short-term and often extremely difficult side effects during or immediately after treatment often takes first priority, it is important to be aware of the types of health problems that may not develop for months or even years. And as the survival rate continues to improve, but treatment still relies on smaller dosages of adult protocols, more and more children will suffer from “late term effects” throughout the remainder of their lives.