Brain Cancers
 Brain cancers account for about 15% of pediatric cancers and are the second most common type of cancer in children. Since the brain controls learning, memory, senses (hearing, visual, smell, taste, touch), emotions, muscles, organs, and blood vessels, the presentation of symptoms varies accordingly.
Brain cancers account for about 15% of pediatric cancers and are the second most common type of cancer in children. Since the brain controls learning, memory, senses (hearing, visual, smell, taste, touch), emotions, muscles, organs, and blood vessels, the presentation of symptoms varies accordingly.
Treatment of pediatric brain cancers (and non-malignant brain tumors) is more complex than is the treatment of some of the other childhood cancers. Surgery to remove the tumor is not always possible, either because the tumor is inaccessible or because surgical removal of the tumor would damage critical parts of the developing brain. Inoperable areas of the brain include the brain stem, thalamus, motor area, and deep areas of gray matter. The prognosis of a brain tumor depends not only on the type, grade, and size of the tumor, but on its location in the brain. Another reason that malignant brain tumors can be difficult to treat is because the blood-brain barrier prevents chemotherapy from entering the brain and reaching the tumor when given systemically.
- More information on the NCI web site: Overview of the diagnosis, classification, treatment, and prognosis of childhood brain tumors – note that you can toggle back and forth between “Health Professional” and “Patient” versions. Also note that the NCI childhood cancer web site links to separate PDQ summaries on brain stem glioma, cerebellar astrocytoma, cerebral astrocytoma/malignant glioma, medulloblastoma, supratentorial primitive neuroectodermal tumors, pineoblastoma, and visual pathway and hypothalamic glioma.
Types of Childhood Brain Tumors
Many different types of brain tumors occur in children, and the nomenclature can seem daunting. Many brain tumors are named for both the type of cell from which the tumor originated and the location of the tumor in the brain. Even the NCI PDQ states that the nomenclature of pediatric brain tumors is controversial and potentially confusing. Properly naming and classifying a tumor is important because proper treatment depends on proper diagnosis. “The pathologic classification of pediatric brain tumors is a specialized area that is evolving; review of the diagnostic tissue by a neuropathologist who has particular expertise in this area is strongly recommended.” (NCI web site, 8/2006) A brief synopsis of brain tumor terminology and descriptions of commonly-named brain tumors follows in the table and paragraphs below.
Examples of Cell Type |
Examples of Location |
General Name |
|---|---|---|
| Primitive neurectodermal, astrocytoma, medulloblastoma, ependymoma | Cerebram, cerebellum, brain stem, optical nerve | Glioma, adenoma, blastoma, carcinoma, sarcoma |
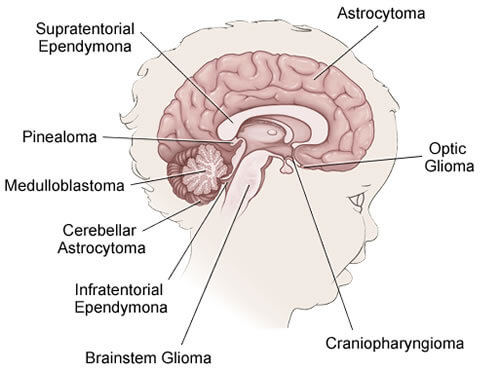
Medulloblastomas arise from primitive neuroectodermal tissue, or PNET. PNET is a general term for a collection of many different brain tumors which arise from undeveloped brain cells. Medulloblastomas are usually located in the cerebellum and are fast growing and highly malignant. They frequently spread, invading other parts of the central nervous system via the spinal fluid. Medulloblastomas account for the largest percentage of pediatric brain cancers. It is more common in boys than girls and usually occurs between the ages of 2 and 6 (only 30% of medulloblastomas occur in adults) and frequently spreads.
Ependymomas arise from the cells that line the internal surfaces of the brain, thus, they are gliomas. The tumors arise from ‘ependyma,’ cells that line the fluid spaces of the brain and spinal cord. Ependymomas located in the cerebral hemispheres occur primarily in children and adolescents. Although these tumors are capable of malignant behavior, they are almost always benign.
Pilocytic Astrocytomas arise from brain cells which form part of the supportive system of the brain, in particular, cells called “astrocytes” for their star shaped appearance. This tumor are usually slow growing and many are considered curable. Astrocytomas are often cystic, in which case they are particularly easy to remove completely.
Optical nerve gliomas are slow growing tumors which form along the optic nerves. They usually occur in children under the age of 10. The common cell type is pilocytic astrocytoma.
Brain stem glioma, located in the brain stem, can be either slow or fast growing. Depending on the type of supporting tissue from which they arise, they can be either astrocytomas, anaplastic astrocytomas, glioblastoma multiforme, or a mixed tumor. In general, brain stem tumors are more common in children than they are in adults. Surgery is usually not possible in these tumors, and radiation and chemotherapy must be used instead.
Oligodendrogliomas are a slow growing tumor which arises from cells which make the myelin that insulates nerve fibers. They are located in the hemispheres of the brain, especially the frontal and temporal lobes, and in children are more common in the thalamus.
Gangliogliomas are usually slow growing, and rarely malignant. These tumors can be located anywhere in the brain, but are most often found in the temporal lobe. They arise from ganglia (a ganglion is a group of nerve cells). They occur most frequently in children and young adults.
Craniopharyngioma are benign (non-cancerous), congenital tumors. They are usually cystic and found primarily in children and adolescents.
Pineal Region Tumors are located in the pineal gland at the posterior portion of the third ventricle. The most common tumor of the pineal region is the germinoma. Germinomas (germ cell tumors) represent over one-third of the tumors in this region. Germinomas of the pineal region are most common in teenagers. Additional tumors found in this area include other embryonal type tumors, teratomas, astrocytomas, pineocytomas, and pineoblastomas.
Symptoms of Brain Tumors
The symptoms depend on the location and size of the tumor. Since the brain controls learning, memory, senses, emotions, muscles, organs, and blood vessels, the presentation of symptoms varies accordingly. Since young children often do not complain of the symptoms, parents must rely on their own observations of their child to be aware of signs and symptoms. Sometimes it is the child’s school teacher who picks up on the signs and symptoms of a child’s brain tumor.
Symptoms can include:
- a seizure not related to high fever
- staring, repetitive automatic movements
- persistent vomiting without any known cause (projectile vomiting), nausea
- progressive weakness or clumsiness; neck tilt, squint
- walking, balance problems
- precocious puberty; growth retardation
- sleep apnea
- vision problems
- headache, especially that wakes the child up at night or is early in the morning
- pain, especially back pain, which should be taken seriously in a child
- changes in personality, irritability, listlessness
As with most childhood cancers, the symptoms of brain tumors are vague and confusing, and are often initially attributed to viruses, neurological problems, or even emotional problems. Most parents of children diagnosed with brain tumors report variations and combinations of the symptoms listed above, symptoms that had no apparent cause and may have lasted for several months before the pediatricians ordered the tests that finally diagnosed a brain tumor.
Treatment for Brain Tumors
Children with brain tumors should be seen at a multi-disciplinary pediatric medical center, staffed with the following team: a pediatric neurosurgeon, a pediatric neuro-oncologist, a pediatric hem-onc, a pediatric neuro-radiolgoist, and a pediatric neuropsychologist. According to the NCI PDQ, radiation therapy of pediatric brain tumors is technically very demanding and should be carried out in centers that have experience in that area in order to ensure optimal results.
Brain tumors are treated with surgery, radiation, and chemotherapy. The specific treatment and prognosis depends on the type, grade, and location of the tumor. Depending on the type of tumor and the promptness of diagnosis, the 5 year survival rate is 40-80%. Long-term management of brain cancer survivors is complex and requires a multi-disciplinary approach.
Where to Find Clinical Trials
The Pediatric Brain Tumor Consortium lists institutions that treat pediatric brain tumors:
The treatment centers listed below under ‘Resources, Web sites’ often list their own clinical trials.
Clinical trials for brain tumors can also be found by searching the clinical trial database on the NCI web site. Follow these directions:
- Start at the NCI clinical trials search page.
- Choose type of cancer: ‘brain tumor, child, type.’ You will be given more choices (e.g., type of cancer and type of trial): choose the appropriate responses and click ‘search.’
Statistics
- 40-80% of the children diagnosed with a brain tumor survive 5 years post-diagnosis
- brain cancers account for 15% of all pediatric cancers
Brain Cancer Awareness Shirt
If you or a loved one has battled brain cancer, if you want to raise awareness, or if you just want to support ACCO, check out our new brain cancer awareness shirts! Available in a variety of apparel, colors, and sizes.
Resources
Book
Websites
- St. Jude Children’s Research Hospital section on childhood brain tumors. Good disease definitions and descriptions and information on treatments.
- MD Anderson Cancer Center Children’s Cancer Hospital– MD Anderson’s website contains information on the symptoms, diagnosis, and treatment of childhood cancers. You can also find information about their Childhood Cancer Survivors Clinic, clinical trials, and BrainSuite.
- The Pediatric Brain Tumor Consortium web site and the American Childhood Cancer Organizations PBTC web page. The PBTC sponsors clinical trials for pediatric brain tumors; the individual institutions that make up the Consortium offer highly informative web sites.
- Virtual Trials. A site managed by the Musella Foundation, a non-profit organization. A lot of information on brain tumors, FAQs, treatment info and options, and a great list of links.
- National Brain Tumor Society The Brain Tumor Society exists to find a cure for brain tumors. It strives to improve the quality of life of brain tumor patients and their families. It disseminates educational information and provides access to psycho-social support. It raises funds to advance carefully selected scientific research projects, improve clinical care and find a cure.
E-mail Support Lists
- ACOR: ped-onc
- ACOR: Medullo-pnet Parents/caregivers/doctors discuss the brain cancers, medulloblastoma and PNET.
- Brain Trust list: Brain Trust list Brain tumors (not pediatric specific)
- Yahoo list: Cerebellarmutism A list of approximately 65 people who share a common interest in these complications from posterior fossa surgery.
- Yahoo list: Pediatric Brain Tumor
More about Childhood Brain Tumor Cancers:
- About Childhood Brain Tumor Cancer – Detection and Diagnosis
- Causes, Risk Factors, and Prevention of Childhood Brain Tumor Cancer
- What are the signs and symptoms of Childhood Brain Tumor Cancer?
- Childhood Brain Tumor Cancer Treatment
- Childhood Brain Tumor Cancer – Stages and Prognosis
- What is the expected life span of Childhood Brain Tumor Cancer?
- After Treatment – Living as a Childhood Brain Tumor Cancer Survivor




