Brain tumors
“What is my child’s prognosis?” This seemingly simple but critical question is often among the first that parents will ask their child’s oncologist after hearing that their child has been diagnosed with cancer. Yet while the question may be simple, answering it can be extremely complicated. In general terms, oncologists can provide statistics relating to 5-year survival rates for many different types of brain tumors in children. These general statistics, however, cannot predict an outcome for any one child. Each child’s individual prognosis will depend on the unique circumstances of their tumor and its response to treatment.
What is a 5-year survival rate and why doesn’t it tell the whole story? The 5-year survival rate refers to the percentage of children who live at least five years after they have been diagnosed with a brain tumor. As a simple statistic, it can provide some basic information about our ability to treat many different types of brain tumors. However, as with all “simple statistics”, it has three significant limitations:
- It only takes into account children who were treated at least five years ago. It does not take into account significant improvements in today’s treatment options.
- It can indicate prognosis for a particular class of brain tumors, but does not show differences in prognosis rates for specific tumor types.
- It does not account for each child’s unique diagnosis and key prognosis factors so, as noted above, it cannot predict an outcome for any one child.
 What are the key prognosis factors for childhood brain tumors?
What are the key prognosis factors for childhood brain tumors?
As noted above, while five-year survival rates can be useful in general terms, each child’s prognosis will depend heavily on a unique assessment of her or her prognosis factors. These factors will impact the treatment approach and help determine your child’s potential for long-term survivorship.
Key prognosis factors for childhood brain tumors include:
- The type of tumor
- The grade of the tumor, or how quickly it is likely to grow
- The size of the tumor
- The location of the tumor
- Whether the tumor can be removed completely with surgery (if at all)
- Whether the tumorous cells have particular gene mutations
- Whether the tumor has spread to other parts of the brain or spinal cord via the cerebrospinal fluid
- Whether tumorous cells have spread beyond the central nervous system
- The child’s age
- The child’s functional abilities as impacted by the brain tumor
Unlike many other forms of cancer, brain tumors rarely spread to areas of the body outside the central nervous system. Instead, brain tumors can be life-threatening because of the damage they can inflict on the delicate and highly critical tissues of the brain and spinal cord. For this reason, doctors do not use two prognosis factors commonly used when discussing other types of childhood cancers: benign v. malignant and “staging”.
Five-Year Survival Rates for Common Types of Brain Tumors in Children
Based on information from the Central Brain Tumor Registry of the United States (covering children treated between 1995 and 2010), we can provide five-year survival rates for some of the most common types of brain tumors diagnosed in children. As noted above, however, it is important to remember that these statistics do not accurately represent the chances of long-term survival for any one specific child.
- Philocytic astrocytoma: 95%
- Oligodendroglioma: 90% – 95%
- Fibrillary (diffuse) astrocytoma: 80% – 85%
- Ependymoma (including anaplastic ependymoma: 75%
- PNETs (including medullablastoma and pineoblastoma): 60% – 65%
- Anaplastic astrocytoma: 30%
- Glioblastoma: 20%
More about Childhood Brain Tumor Cancers:
- About Childhood Brain Tumor Cancer – Detection and Diagnosis
- Causes, Risk Factors, and Prevention of Childhood Brain Tumor Cancer
- What are the signs and symptoms of Childhood Brain Tumor Cancer?
- Childhood Brain Tumor Cancer Treatment
- Childhood Brain Tumor Cancer – Stages and Prognosis
- What is the expected life span of Childhood Brain Tumor Cancer?
- After Treatment – Living as a Childhood Brain Tumor Cancer Survivor
Learn More About the Different Types of Childhood Cancers:
- Childhood Brain Tumor Cancer (Brain Stem Tumors)
- Spinal Cord Tumor Cancer
- Childhood Neuroblastoma Cancers
- Childhood Hodgkin Lymphoma Cancers
- Non-Hodgkin Lymphoma Cancers
- Wilms tumor (Kidney Tumors)
- Rhabdomyosarcoma
- Retinoblastoma
- Bone cancer (including osteosarcoma and Ewing sarcoma)
- Leukemia Cancers: Acute lymphocytic (lymphoblastic) leukemia (ALL) Acute myelogenous leukemia (AML); Juvenile myelomonocytic leukemia (JMML)
- Hepatoblastoma (Liver Cancer)
- Rhabdoid Tumors
About American Childhood Cancer Organization
American Childhood Cancer Organization (ACCO) is a non-profit charity dedicated to helping kids with cancer and their families navigate the difficult journey from cancer diagnosis through survivorship. Internationally, ACCO is the sole U.S. member of Childhood Cancer International (CCI), the largest patient-support organization for childhood cancer in the world. Here in the United States, ACCO promotes the critical importance of ensuring continued funding into new and better treatment protocols for childhood cancer. And most importantly, ACCO is focused on the children: developing and providing educational tools for children fighting cancer and their families, empowering them in their understanding of childhood cancer and the medical decisions they must make during this difficult journey. All of ACCO’s resources are available free of charge for families coping with childhood cancer.
For additional information about childhood cancer or on the ACCO, or to order resources for you or your child, please visit our website at www.acco.org , call 855.858.2226 or visit:
 When classed together in a single grouping, cancers in the brain and spinal cord are the second most common type of childhood cancer after leukemia. Brain and spinal cord tumors account for about 25% of all childhood cancer diagnoses, with more than 4,000 new cases diagnosed every year in the United States. In reality, however, it can be difficult to discuss “brain tumors” in general terms: oncologists recognize at least nine different sub-classifications of brain tumors in children, such as brain stem gliomas and ependymomas for example, with still more sub-groupings within those broad classifications.
When classed together in a single grouping, cancers in the brain and spinal cord are the second most common type of childhood cancer after leukemia. Brain and spinal cord tumors account for about 25% of all childhood cancer diagnoses, with more than 4,000 new cases diagnosed every year in the United States. In reality, however, it can be difficult to discuss “brain tumors” in general terms: oncologists recognize at least nine different sub-classifications of brain tumors in children, such as brain stem gliomas and ependymomas for example, with still more sub-groupings within those broad classifications.

 Grace loves to be crafty; she made a sign for the children to sign and date which says “Last Day of Chemo.” Throughout her treatment, she decided to paint pictures to brighten the nurses and the children’s days. When losing her hair became a reality, Grace decided to throw a party and shave her head. Grace’s brother and her best friend joined her in shaving their heads as well.
Grace loves to be crafty; she made a sign for the children to sign and date which says “Last Day of Chemo.” Throughout her treatment, she decided to paint pictures to brighten the nurses and the children’s days. When losing her hair became a reality, Grace decided to throw a party and shave her head. Grace’s brother and her best friend joined her in shaving their heads as well. lking to people about this part of her journey and is focused on helping others. Grace plans on learning more about oncology. She is excited for the future and can’t wait for her hair to start growing back!
lking to people about this part of her journey and is focused on helping others. Grace plans on learning more about oncology. She is excited for the future and can’t wait for her hair to start growing back!  Any time a child is diagnosed with a brain tumor or other type of cancer, the most obvious question many parents ask is “why”. What caused this child to develop a brain tumor? Unfortunately, there is no easy answer to this question. Scientists now believe that the vast majority of brain tumors in children are the result of random gene mutations but have no satisfying answer as to why a particular gene mutation occurred or why it led to the growth of a brain tumor.
Any time a child is diagnosed with a brain tumor or other type of cancer, the most obvious question many parents ask is “why”. What caused this child to develop a brain tumor? Unfortunately, there is no easy answer to this question. Scientists now believe that the vast majority of brain tumors in children are the result of random gene mutations but have no satisfying answer as to why a particular gene mutation occurred or why it led to the growth of a brain tumor. After leukemia, brain tumors (including spinal cord tumors) are the second-most common type of cancer in children, accounting for about 25% of all childhood cancer diagnoses. Brain tumors begin within the delicate and complicated tissues of the brain or the cerebrospinal fluid (as well as the spinal cord or central nervous system, as these tumors are usually classed with brain tumors in children). When dealing with brain tumors in children, oncologists rarely differentiate between benign (non-cancerous) or malignant (cancerous) tumors; all tumors in the brain can be life-threatening whether technically cancerous or not. Instead, oncologists usually focus on how fast the tumor is growing, how quickly or easily it may spread throughout the brain or spinal cord, and how easy the tumor is to remove completely.
After leukemia, brain tumors (including spinal cord tumors) are the second-most common type of cancer in children, accounting for about 25% of all childhood cancer diagnoses. Brain tumors begin within the delicate and complicated tissues of the brain or the cerebrospinal fluid (as well as the spinal cord or central nervous system, as these tumors are usually classed with brain tumors in children). When dealing with brain tumors in children, oncologists rarely differentiate between benign (non-cancerous) or malignant (cancerous) tumors; all tumors in the brain can be life-threatening whether technically cancerous or not. Instead, oncologists usually focus on how fast the tumor is growing, how quickly or easily it may spread throughout the brain or spinal cord, and how easy the tumor is to remove completely. Meet Pedro, a 5-year-old warrior turning 6 this December. Pedro is one of three children in the Curiel family and is suffering from T Cell Acute Lymphoblastic leukemia (ALL). He is receiving delayed intensification treatments in California with his mom and siblings by his side.
Meet Pedro, a 5-year-old warrior turning 6 this December. Pedro is one of three children in the Curiel family and is suffering from T Cell Acute Lymphoblastic leukemia (ALL). He is receiving delayed intensification treatments in California with his mom and siblings by his side.  When he’s not receiving treatment, he is found drawing treasure maps around the house. Vilma said that he loves to draw these maps and hide his “treasure” and have his two brothers go find it! He started homeschooling in August, and he can now read a full sentence. He is expected to return to school after flu season.
When he’s not receiving treatment, he is found drawing treasure maps around the house. Vilma said that he loves to draw these maps and hide his “treasure” and have his two brothers go find it! He started homeschooling in August, and he can now read a full sentence. He is expected to return to school after flu season.  announcement of its new global initiative to address the disparity between childhood cancer survival in low-middle versus high-income countries. The announcement came at the United Nations (UN) General Assembly’s side-meeting on childhood cancer
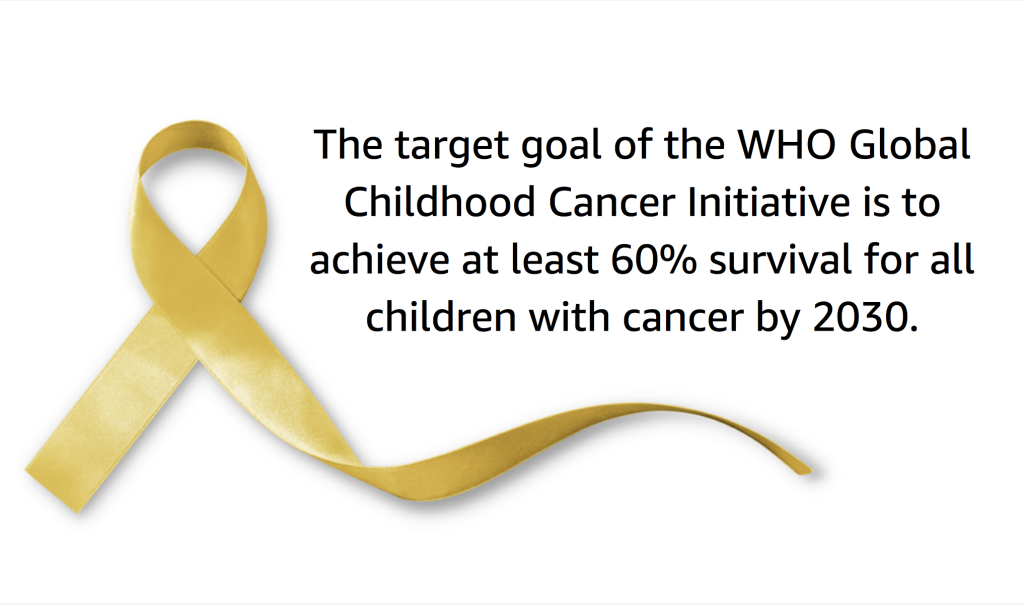
announcement of its new global initiative to address the disparity between childhood cancer survival in low-middle versus high-income countries. The announcement came at the United Nations (UN) General Assembly’s side-meeting on childhood cancer 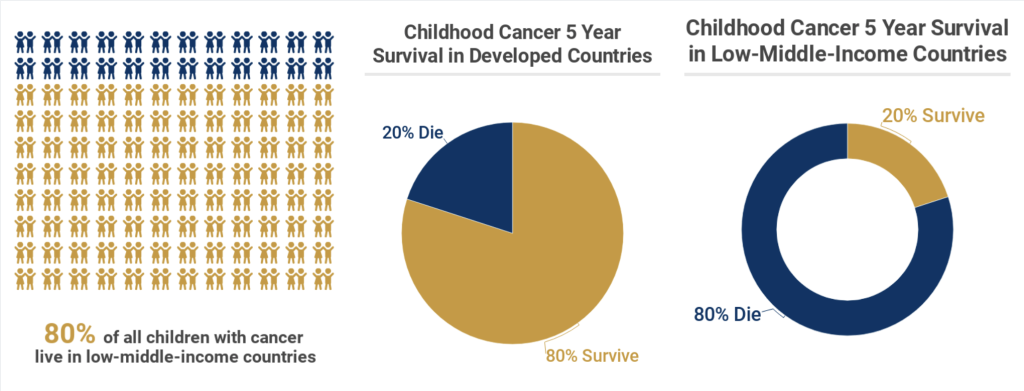
 Meet Beckham, one of our ambassadors for the month of September. He is a goofy 8 year old currently being treated for Stage 4 Neuroblastoma at Memorial Sloan Kettering in New York City. Beckham was diagnosed on September 11, 2013 at the age of 3. A few weeks prior to his diagnosis, Beckham was playing with his sister and they banged their heads together. This resulted in Beckham’s black eyes. His mom remembers looking at pictures from that time and seeing his eyes starting to darken.
Meet Beckham, one of our ambassadors for the month of September. He is a goofy 8 year old currently being treated for Stage 4 Neuroblastoma at Memorial Sloan Kettering in New York City. Beckham was diagnosed on September 11, 2013 at the age of 3. A few weeks prior to his diagnosis, Beckham was playing with his sister and they banged their heads together. This resulted in Beckham’s black eyes. His mom remembers looking at pictures from that time and seeing his eyes starting to darken.  At first, doctors didn’t think Beckham had cancer, they went through many diagnoses, everything from mono to anemia. The doctors were not convinced and decided to do a bone marrow biopsy which revealed that Beckham had tumors throughout his body and bone marrow.
At first, doctors didn’t think Beckham had cancer, they went through many diagnoses, everything from mono to anemia. The doctors were not convinced and decided to do a bone marrow biopsy which revealed that Beckham had tumors throughout his body and bone marrow.  Treatment was aggressive and as a result Beckham started chemotherapy. The doctors performed a resection of the main tumor and radiation to his skull in Utah which resulted in soft tissue tumors and bone marrow clearing well but the tumors in his bones had hardly changed. Beckham’s mom recalls going onto a Facebook group for Neuroblastoma and was urged to take him for a second opinion at Memorial Sloan Kettering. February 2014 was the first trip to NYC where Beckham received MIBG therapy, NK cell therapy, radiation, 3f8 antibioties, cryotherapy surgery, numerous rounds of chemotherapy and surgery to remove lymph nodes in his upper right underarm and chest.
Treatment was aggressive and as a result Beckham started chemotherapy. The doctors performed a resection of the main tumor and radiation to his skull in Utah which resulted in soft tissue tumors and bone marrow clearing well but the tumors in his bones had hardly changed. Beckham’s mom recalls going onto a Facebook group for Neuroblastoma and was urged to take him for a second opinion at Memorial Sloan Kettering. February 2014 was the first trip to NYC where Beckham received MIBG therapy, NK cell therapy, radiation, 3f8 antibioties, cryotherapy surgery, numerous rounds of chemotherapy and surgery to remove lymph nodes in his upper right underarm and chest.  Beckham has had two central lines and is on his third port. “He has endured four relapses, the most recent being March of 2018 and his doctors say he is a miracle boy.”
Beckham has had two central lines and is on his third port. “He has endured four relapses, the most recent being March of 2018 and his doctors say he is a miracle boy.” 


 Fortunately, Braeden is facing treatment like a little soldier; the only side effect he has experienced was hair loss, which he doesn’t seem to mind. Kendra notes that everytime he goes into the hospital, the nurses fight to work with him and that he charms them. She said when Brae is at home, he loves to watch tv with his big brother and play outside. He’s particularly interested in art and loves to paint. When he goes to the hospital you can usually find him in the art room playing with the popsicle sticks and paint.
Fortunately, Braeden is facing treatment like a little soldier; the only side effect he has experienced was hair loss, which he doesn’t seem to mind. Kendra notes that everytime he goes into the hospital, the nurses fight to work with him and that he charms them. She said when Brae is at home, he loves to watch tv with his big brother and play outside. He’s particularly interested in art and loves to paint. When he goes to the hospital you can usually find him in the art room playing with the popsicle sticks and paint.  There are nearly 5,000 new diagnoses of childhood leukemia every year in the United States, making this so-called “rare” disease the most common type of childhood cancer. In fact, childhood leukemia currently accounts for almost one-third of all childhood cancer diagnoses. Thanks to amazing advances in the efficacy of today’s treatment protocols, the majority of children diagnosed with leukemia today can expect to make a full recovery. The 5-year survival rates for the two main forms of leukemia—Acute lymphocytic (lymphoblastic) leukemia (ALL) and Acute myelogenous leukemia (AML)—are greater than 85% and about 60-70% respectively.
There are nearly 5,000 new diagnoses of childhood leukemia every year in the United States, making this so-called “rare” disease the most common type of childhood cancer. In fact, childhood leukemia currently accounts for almost one-third of all childhood cancer diagnoses. Thanks to amazing advances in the efficacy of today’s treatment protocols, the majority of children diagnosed with leukemia today can expect to make a full recovery. The 5-year survival rates for the two main forms of leukemia—Acute lymphocytic (lymphoblastic) leukemia (ALL) and Acute myelogenous leukemia (AML)—are greater than 85% and about 60-70% respectively.